
The transcription below is from my presentation at the Sound Stimulation session at the TRI 23 Conference in Trinity College Dublin on June 8th 2023. It has been edited to remove all the “ums”, “ahs”, “you knows” and the other vocal tics that transcribing software reveals to you.
Prof Dirk De Ridder- Clinician Researcher, University of Otago: Now it’s a pleasure to invite Brian Cleary for a very important talk on cochlear implantation for single sided deafness and severe tinnitus – the patient perspective. Brian is a pharmacist and a researcher, and, being implanted, he can give us a perspective that we normally can’t have. Being a researcher himself can also help us in suggesting what, from the patient’s perspective, is very important for us for further research. So, let’s all put our hands together and thank Brian that he’s willing to give this up his time for this.

Brian Cleary: Many thanks! You are all very welcome to Dublin. I went to college here and it’s great to be back.
So, as Prof De Ridder said, I am the Chief Pharmacist in a maternity hospital and I work with the School of Pharmacy and Biomolecular Sciences at the Royal College of Surgeons, where I’m an Honorary Clinical Professor. In terms of conflicts of interest: I have hearing loss;
I’m a patient advocate, so I try and make as much noise as possible and work at raising awareness about sudden hearing loss and trying to improve access to treatments for patients; I have a website that advocates for that; and I’m a cochlear implant recipient. I don’t monetize the website. I don’t receive anything from companies that have commercial interests in this space.
Some background: I’m married with three children and we have a lot of fun. This is over on the West Coast over near the Cliffs of Moher that were onscreen yesterday. Music is very important to me. Our house is filled with instruments and I play a lot at home and sometimes with friends at sessions around Dublin.
I work in the Rotunda, the oldest, continuously operating maternity hospital in the world. It was founded before a lot of countries, opening in 1745 and moving to its current location in 1757, a couple of years before Arthur Guinness set up his establishment.
I’m usually in your position. I’m usually at the conference as a participant. I supervise research, I supervise PhD students. I publish in the area of pharmacoepidemiology, looking at use of medications in large populations, particularly around safe and effective use of medicines in pregnancy.
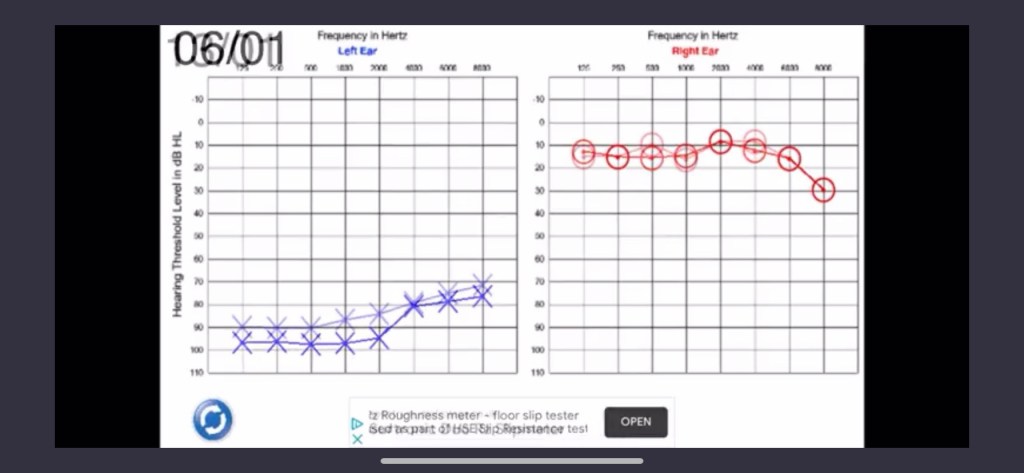
This is my audiogram. I woke up on the 26th of December, 2021 with with a sense of fullness and no hearing in my left ear. I went through standard treatment. I got oral and intratympanic steroids and 30 sessions of hyperbaric oxygen treatment. There was a slight improvement, but I remained in the profound hearing loss territory.
I think storytelling is important. I think we need to hear patient stories. I thought this before I became patient. So, you know, instead of telling everyone at work that I wouldn’t be back for a little bit as I was getting treatment, I just told everyone via Twitter.

Here you can see how kids dressed me up as Vincent Van Gogh with my bandaged ear. So, I used that micro blogging approach to document the experience over time, to share the story, and to try and see, you know, is there a way to help one person in a similar situation? Is there someone out there who will read this and who will get better care as a consequence? Is there some health professional who will think about sudden sensorineural hearing loss in their differential diagnosis when people present with hearing loss? That evolved into something a little bit bigger and a therapeutic writing exercise. I was keeping a diary at the time, so I set up a blog called Noisy Silence.

Essentially the posts address each of the successive parts of that journey as I went through the initial sudden hearing loss, the steroid and hyperbaric treatment, getting back out there after treatment hadn’t worked and also the process of getting back to work/working with single-sided deafness.
Tinnitus emerged over time and became a big feature of my story. I remember the initial days when I just had silence on the left. Listening to music via headphones, the left side of the mix was missing. I have a blog post called Tinnitus Talk. It was named for the podcast because I found it very useful. Some of the people at this conference were involved in excellent episodes. My tinnitus wasn’t there straight away. So I was very interested in hearing about the top-down and bottom-up models of tinnitus and thinking about how they chime with my experience. Listening to songs on headphones, I had a completely blank left channel immediately after my hearing loss. So listening to the Beatles, all of the left side is gone. So the guitar intro from Here Comes the Sun disappears.
If you fast forward a few months, my tinnitus responded to the noise environment I was in. So, if I listened to music, the tinnitus just got louder, never to be outshone by the music. It got louder if I was in a noisy environment. If I was up in that space where the reception was last night, that reverberant, loud space, it just fed the tinnitus and it would get that loud that I just had to get out of that space or avoid some scenarios. So there’s definitely a period of avoidance with tinnitus and hyperacusis.

Ultimately, I stepped back a little bit from work, moving to a four day week, got counseling through my employee assistance program, and came up with healthy coping strategies to try to prevent the potential adverse mental health effects that I knew were possible with severe tinnitus.
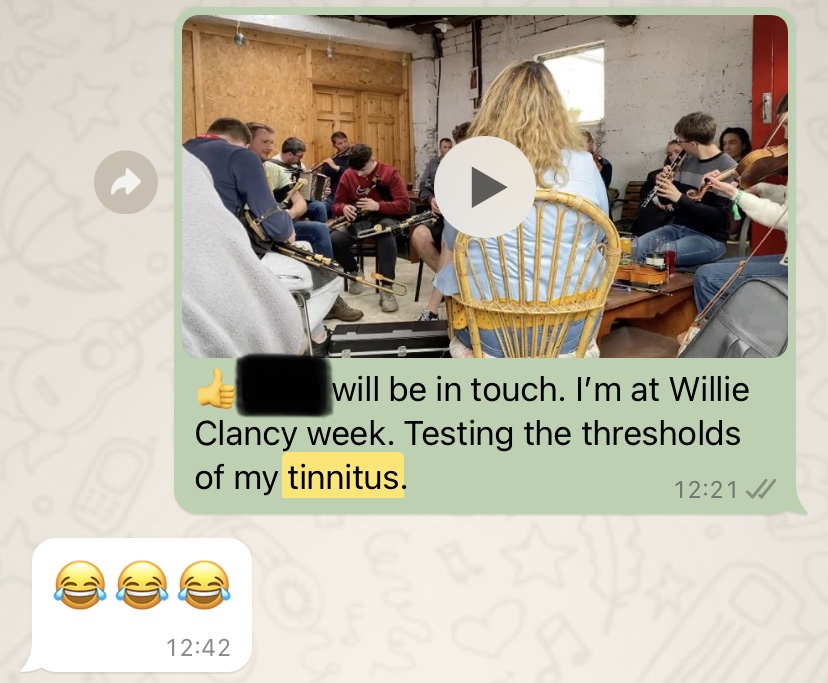
This is a picture from the Willie Clancy Festival from West Clare. This traditional Irish summer school and music festival attracts people from around the world to learn how to play uileann pipes, tin whistles, fiddles and other traditional instruments. This is a nightmare for someone with tinnitus, but you have to get out there and you have to try not to fall into avoidance behaviours, which may get worse with time. So here I’m just texting a friend about pushing the tinnitus as hard as I can to see how loud can it get.
I did have a tinnitus matching test done as part of the CI workup. The audiologist came up with a broadband sound that emulated my tinnitus. I listened to this in my good ear and flagged when the volume matched the tinnitus volume in my bad ear. My tinnitus involved white noise with some individual tones too across a range of frequencies. There were times, with excessive, sound input, such as a long car journey, that I got the sound of an anvil being hit with a hammer.
That was quite rare. Essentially, she matched the usual tinnitus sound and started increasing the volume. She got up to eighty three decibels before it matched the tinnitus sound in my left ear. So, that was after I’d done some audiometry and the sound input from the audiometry had fed the tinnitus and it made it louder. When I explained the volume to people, I said that it is like you wake up in the morning and someone hands you a hair dryer, and you carry that around with you all day. If you’re in a loud environment, the hairdryer is on the highest setting. If you go into a quiet environment, it might slowly drop down to the lowest setting, but it’s still a hair dryer at arm’s length for every conversation and thought that you have. So, there was a need to seek silence due to this form of reactive tinnitus, or crossover tinnitus, as some of the people in the sudden sense hearing loss/single-sided deafness community refer to it.

I came up with healthy coping strategies: lots of walks, lots of swimming, trying to avert the potential mental health effects. This little lady accompanied me on lots of walks all over the countryside and up and down beaches everywhere. To seek silence, I had to advocate for myself as there was no access to cochlear implantation for single-sided deaf patients in the Irish Health system. We’ve got one national public CI service and it’s busy with bilateral deafness and pediatric cases, and those are definitely people who should be prioritized.
I use my literature search and critical appraisal skills to present the evidence base for cochlear implants to restore binaural output and reduce the impact of tinnitus and tinnitus-related distress.
I saw the various cases series, starting with the initial work from Belgium back in 2008 up to and including some RCTs and a Canadian Health Technology assessment that basically, found that CI for SSD was cost effective. (Note– in checking through the transcription afterwards, I had a look at that original Belgian paper from 2008 and Prof. De Ridder who introduced me at this session was senior author on that paper 🤯. I wish I had known at the time, as this paper had a major impact on my life)
I was 41 when this happened and I have, potentially, 25 years left in my working life based on the Irish retirement age, which is creeping upwards. So it made sense for this to be paid for, but they refused previous applications and no one had gotten through the process. I don’t know was it the evidence summary or what, but they accepted my application. So the precedent was set and now there are several patients in my situation coming after me that I’m helping go through the process.
The process involves the European Union Treatment Abroad Scheme, which basically, because of EU freedom of movement, gives you the right to access equivalent treatments that other EU citizens can access. So if single-sided deafness is covered in the German health system or the Spanish health system, or another jurisdiction within the EU, you can apply through this scheme to access the treatment. The referring health system gets the service at public patient costs in the host country. The health system then pays the host country through an intermediary like an insurance company.
So Noisy Silence now has 13 posts up. It’s long form, and it’s what I was looking for. I wanted a long article describing what it was like with SSD, dealing with tinnitus, getting a CI, and going through the adjustment/rehab process. I wrote it for myself with the kind of information I needed. It’s approaching about 3000 views now from about 1200 visitors. The initial post Dawn of the Deaf has 240 views, the latest post the wall has 127. So some people are getting all the way through the 13 posts. I get a lot of great feedback from people on Twitter and directly via email.
There’s quite a broad, geographical spread, although it’s mostly anglophone countries.

I had to go to Berlin for the CI. Of the potential EU countries, Germany worked best. I speak some German. I could get to Berlin reasonably easily as I live near the airport. Now, I also live about a 20 minutes walk away from the Irish CI Center, so it might have been a little bit easier to get to there. I had to drive home from Berlin because the recommendations from the center are to avoid flying immediately after the surgery. So that made life a little bit complicated.

I had plenty of time on that drive to Berlin to think about what does good look like. I was hoping for: some return of binaural hearing; greatly diminished tinnitus when I wear the implant; reversal of some of the things that tinnitus strips away: being able to hear my children and family, not having sound sensitivity and hyperacusis when children are being children, and to have less tiredness at the end of the day- all that listening fatigue- you get to the end of the day at work and you go home and there’s nothing left in the battery, and then less grouchiness or less time and energy spent consciously trying not to be grouchy; and then some of the things I missed out on as a consequence of tinnitus and hearing loss: trying to get out there socially, spend more time playing music, spend more time seeing people because with COVID, I had to isolate to access hyperbaric treatment, to get over for the pre-op assessment and for the surgery- if you had covid on the pre-surgery checks, you would be turned back and sent home, so there are a lot of implications in terms of isolating. Luckily, I’m fortunate to be able to say that I got all these things and more. I’ve got greatly diminished tinnitus as a consequence of the CI and it has been completely life-changing. Although I still have the slightest tinnitus that I can only hear if I look for it when it’s silent, I no longer have any tinnitus related suffering.
Thinking about some of the opportunities, research questions, and novel approaches from being a patient observer so far at this conference, I have some rough ideas outlined here. Firstly, I want to second everything that, Nic Wray from TinnitusUK said in the session earlier today. That group as an organization are very good at listening to patients and giving the patients a voice. I’d like to add the following points or questions or potential research questions:
Why did I lose my hearing? What was the trigger? 90% of cases of sudden sensorineural hearing loss are idiopathic (unknown cause) despite fairly extensive investigations. How can we reduce this huge degree of uncertainty?
Why isn’t there better public and health professional awareness of sudden sensorineural hearing loss? The vast majority of people who contact me, who are in a similar situation, have delayed diagnosis or did not have access to effective treatment. They’re not getting in to see health professionals quickly enough, and they’re not getting to an ENT specialist who can potentially get them treatment that might save their hearing.
How can we amplify the messages of hearing loss charities, like Tinnitus UK and Chime in Ireland?
Can we try to to get more prospective enrollment and open science? Unfortunately, there’s a constant supply of patients in my situation. They’re appearing on the single sided deafness forums and sudden hearing loss forums all the time. There should be enhanced opportunities for patients to participate in research. It should be the default. Research participation should be a right for patients and it should be routine because that’s what happens in other disease states and that’s how we push things forward.
I’m looking for enhanced collaboration between researchers. We should be looking at common research frameworks, we saw a national assessment of an intervention, with a collaborative model using standardised protocols across South Korea just before my talk. I’m involved in some research to assess an intervention to reduce the risk of peripartum adverse outcomes. This will need a trial with 20,000 participants that will be done across multiple countries. By each study using a common protocol, individual patient data meta analysis can be used to combine those different jurisdictions with everyone working off the one protocol. So, you know, can we develop good protocols in this context? Can we get everyone singing off the same hymn sheet and reduce research waste?
How do we build a learning health system, so that we can integrate research into clinical practice? Can we learn from every patient that goes through the system, so it feeds into an ongoing knowledge pool that can be drawn on to find patients like me, and to tell me on day one, these are the potential outcomes, this is what we’re going to do to improve your chances. These routinely collected data can also be used to advocate for better funding for research and the enabling infrastructure. Looking at the relationship with industry, and it’s important that it’s there, but it needs to be configured appropriately and always needs to be clearly declared. You need to look at patient and public trust in the process to ensure that there aren’t scandals, like those that have happened in other fields.
Implementation science- how do you implement the interventions that we know clearly work? There have been so many talks about CBT, with some work going back decades and yet it still isn’t routinely accessible. Some interventions seem stuck forever in the assessment phase instead of moving to implementation at scale.
People in my situation are perfect human tinnitus models. I get frustrated when tinnitus is referred to as a single entity when it’s really a common symptom for a diverse bunch of people. I wholeheartedly agree with the earlier speaker. Precise phenotypes please. I am not the same as someone with mild to moderate tinnitus that they can mask. I look at tinnitus resources that tell me to mask the tinnitus. I’m talking in a sound therapy session here today, but I had no hearing for masking or sound therapy. Sound actually made the tinnitus worse for me. So there are definitely tinnitus subtypes. Some of them are probably very rare and may not be generalizable, but carefully delineating them might help in terms of aetiological clues and giving a sense of potential targets for intervention.
So, can we prospectively follow what’s going on when that patient loses their hearing suddenly? They’re probably going to develop quite severe tinnitus- that should also be carefully studied over time. People like me, we have an on off switch, we can be studied and objective measures of tinnitus severity and quality can be developed with us as a patient group. How do we prospectively evaluate people? The earlier talk about immediate CI activation (around 24 hours after surgery) was very interesting. My tinnitus was terrible in the first 24-48 hours after the surgery, and I felt it was positional. I was thinking of fluid leaking from the inner ear and the potential effect of of that on the tinnitus, but it improved slowly for me prior to activation. When I went to return my hearing aid to my audiologist prior to activation, they felt that placement of that CI electrode array could have affected some process that may have softened the tinnitus.in my experience, since activation, sound kills tinnitus. This was quite soon (minutes after activation for me. I went back to the hotel room after exposure to traffic noise and the chatter of my family in the first half hour to forty minutes after activation and I heard silence for the first time in a year. It doesn’t make sense to me that it’s that quick in light of all of the neuroplasticity and things are being discussed at this conference, but, in my experience, sound kills tinnitus. It is still there for me if I sit in silence and listen out for it. I hear a very subtle version of it. But are there potential approaches where get sound exposure all the time to complete eradicate the tinnitus? I have seven to eight hours off the CI every night. My brain listens all that time. Obviously I’m listening, as I can hear my alarm when I need to wake up in the morning. So Is there potential to eradicate that remaining tinnitus with more sound exposure songs throughout the night? I only have one processor and I don’t want to try it, but someone should consider it.
The qualitative lived experience of people with severe tinnitus: how do you document the stories of this patient group? You know, you can quote all the health economics arguments, you can quote all the study findings and data that you like they’re really important, but without the patient’s stories, you won’t get everyone on board to bring about change.
Inner ear therapeutics is potentially fantastic stuff. I saw an impressive micro needle poster out there earlier. Really cool stuff. But please don’t over hype inner ear therapeutics because there are patients turning down effective currently available interventions because of overhyped, potential future treatments, many of which are falling at various phases of the drug development process. clinical trials stages.
Involve the public and patients more. There could have been more public and patient involvement. yesterday and today. It’s great that there’s an event tomorrow and I think you’re heading in the right direction as a group, but patients could have a very positive impact on the field. There’s great potential for patient reported outcome measures to improve outcome measurement. The digital healthcare talk this morning, really points to your potential in that space and opportunities to activate the wider tinnitus community.
From a public awareness perspective, there are untapped resources out there. There are big names out there with severe tinnitus. How can we get them to become advocates?
And finally, including patients in priority setting from a research perspective, research design and moving towards open science principles using patient reported outcomes and digital healthcare. There are API’s there that would enable third party apps like some of what’s being presented earlier, to integrate with electronic health records, APIs like SMART on FHIR have been used in other contexts to do this. That information will then become routinely available for epidemiological and other research and for the implementation science piece. How do we get the things that we know work out there so that patients can access them?
So that’s it, thanks for listening. That’s my Twitter handle and that’s the QR code for noisysilence.ie